Sensory Processing Disorder Parent Support
What is Sensory Processing Disorder? (SPD)
Children with sensory differences ... painting the world beautiful.
What is Sensory Processing Disorder? (SPD)
Jeanette Loftus
A child who struggles with sensory processing disorder can have difficulty with the sensory unput around them in their environment. It can be difficult for them to live with sensory processing disorder because it can feel very overwhelming.
Studies on sensory processing disorder indicate that 5–16% of individuals have sensory processing differences. It can be very challenging for someone to engage in everyday duti es when they have difficulties with sensory processing.
How many children struggle with Sensory Processing?
One study suggests that 1 in every 6 children experiences differences in sensory processing that may be significant enough to affect aspects of everyday life functions.
(Ben Stasson , Carter, Briggs-Gowen, 2009)
A study from 2004 showed that at least 1 in 20 children’s lives are affected by sensory processing disorder.
(Ahn, Miller, Milberger, McIntosh)

What are the ris k factors for SPD?
Several groups ( Ben Stasson ) et al., 2009; Keuler et al., 2011; May-Benson et al., 2009; Schneider et al., 2007, 2008, 2009; Wickremasinghe et al. in press;) suggest the following are possible risk factors associated with SPD:
Low birth weight (less than 2200 gram
Prematurity (less than 36 weeks ge station)
Prenatal complications
Maternal stress
Maternal illness
Maternal use of medications
Delivery complications
Assisted delivery methods
Ethnic minority
Living with a single parent
Lower socioeconomic status
How Does Sensory Processing Disorder Impact Daily Life?
Sensory processing disorder can cause a lot of different difficulties like getting dressed, eating or attending large social events can be overwhelming for those with sensory challenges. These struggles can often affect our work, friendships, relationships and our life at home too.
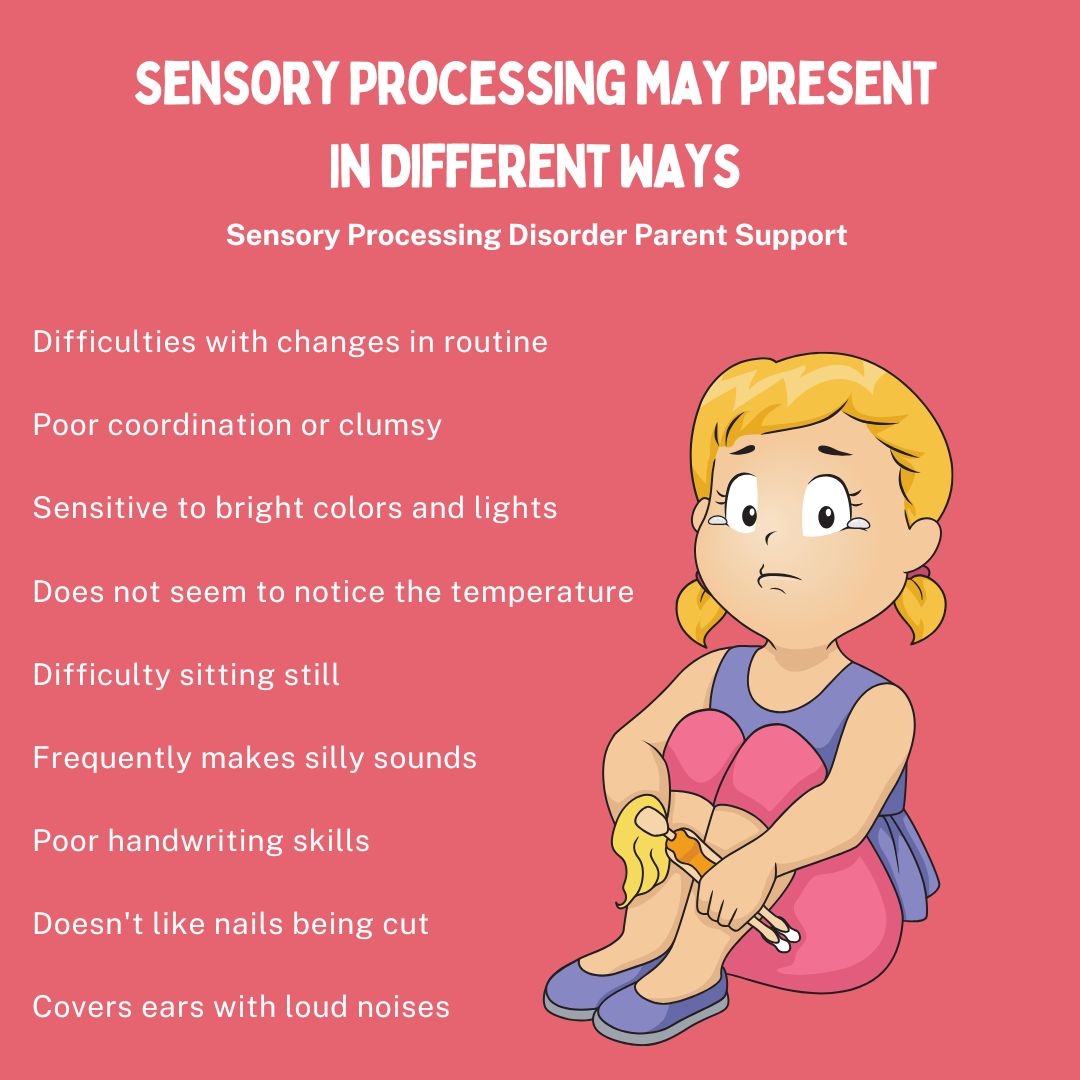
Common Symptoms of Sensory Processing Disorder
Each person who has sensory processing disorder may experience a lot of different symptoms as it is so different for everyone. A person who struggles with sensory processing may be hypersensitive (over-responsiveness) or hyposensitive (under-responsiveness) to sensory input. A person with hypersensitivity might feel that some textures unbearable, while someone with hyposensitivity might seek out intense sensory experiences.
Your child may be struggling to cut their nails, wash their hair, dress themselves, have difficulties with balance or they may have difficulties with their fine and gross motor skills. They could become upset by loud noises or have trouble focusing. Some children struggling with food and eating. These could all be possible symptoms of sensory processing disorder. Please check the sensory checklist for more common symptoms of sensory processing disorder.
Types of sensory input
We have 8 sensory systems, they all contribute to our daily functioning and engagement with the world. Some of these systems are more ‘known’ and others may be new for you.
1. Tactile-what you feel (touch).
2. Visual-what you see.
3. Auditory-what you hear.
4. Gustation-what you taste.
5. Olfactory-what you smell.
6. Proprioception-body awareness. This is the ability to know where you are without using your sight. If you close your eyes and touch your nose successfully that’s because of your proprioceptive system.
7. Vestibular-where you are in space, this input comes from movement and head position. Your vestibular system lets you know if you are upright or hanging upside down.
8. Interoception-how you ‘feel’. This is input that lets you know you are hungry, thirsty, need to use the restroom, that your heart is beating fast, that you are hot or cold, etc.
It’s the input we receive from these 8 systems constantly during our day that our brain is receiving and interpreting. Some people may be under-responsive to input, others may be over-responsive.
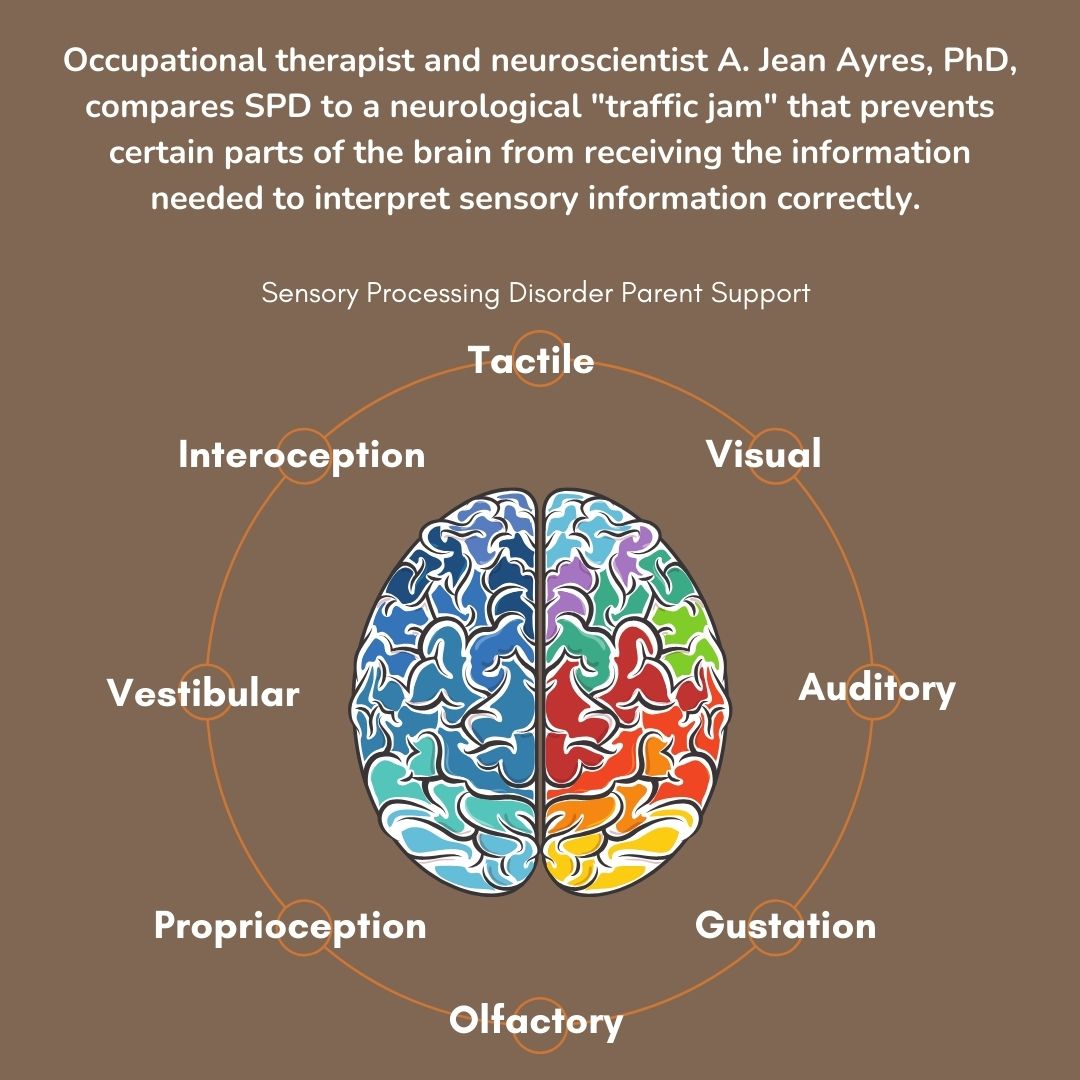
Occupational therapist and neuroscientist A. Jean Ayres , PhD, compares SPD to a neurological traffic jam that prevents certain parts of the brain from receiving the information needed to interpret sensory information correctly.
Coping with Sensory Processing Disorder
There are therapies, tools and strategies to help cope when you are living with sensory processing disorder. Occupational therapy and modifications in a person's daily life are common ways to support individuals who are struggling with sensory processing disorder.
Creating a sensory-friendly environment and developing coping skills can help an individual who lives with sensory challenges be able to cope better and stay regulated.
Hypersensitive and Hyposensitive
Hypersensitive means that you are more sensitive (over-responsive) to input than others. This may look like covering your ears when a vacuum is turned on because it is too loud. Or struggling with the feeling of your clothing, even to the point of not being able to wear clothes. At times we refer to people that are hypersensitive as avoiders, they want to avoid certain types of input because they are more sensitive to them.
Hyposensitive means that you are less sensitive (under-responsive) to input than others. Meaning you may want and crave more input to feel regulated and fulfilled. This may look like constantly moving, spinning, jumping, or playing rough with others. At times we refer to people that are hyposensitive as seekers.
It is not uncommon for someone to be both hypersensitive and hyposensitive at the same time. This can change day-to-day as well. For example, someone may be hypersensitive to touch and struggle with the texture of their clothing but be hyposensitive to proprioceptive input and seek out more rough play and heavy work where their muscles are being engaged.

Sensory Processing Disorder can be ... Sensory Seeker symptoms & sensory avoider symptoms or both.
Treatment for Sensory Processing Disorder is a sensory diet, a sensory diet are sensory activities that are scheduled throughout the day, everyday to help a person learn to process sensory input and improve their regulation.
An occupational therapists (OT) that specializes in sensory processing disorder and can help you set up sensory diet for your child and help support you when treating your child's sensory processing disorder. You can request a referral from your pediatrician or family doctor.
Your child's occupational t herapist will complete an evaluation and start a sensory diet for your child that are for your child's sensory needs.
Sensory Processing Disorder can have a significant impact on someone and their family. If you suspect that you or your child may be struggling with sensory processing disorder, seek help and support from a pediatric occupational therapist or pediatr ician.
Resources For Parents
Kids Sense Sensory Processing Disorder (SPD) - Kid Sense Child Development
DISCLAIMER: I have learned a lot over the years but I am still learning. Always do your own research and exercise sound judgment. I am not an occupational therapist or a physician. I am an adult who has sensory processing disorder, a sensory parent and a Grandma. The information on this website is not medical advice and does not replace the information that your child's therapists or medical professionals give you. These are just ideas that I have learned myself over the years of being a parent and an adult living with SPD. If you are concerned for your child, please always seek medical attention through a family doctor, pediatrician or therapist. This website is for awareness purposes only. Each child is different and what works for one child may not for another because all children have different sensory needs. Please always consult with a medical professional. C lick on links throughout each page for more resources and information. Click here for more resources https://sensoryprocessingdisorderparentsupport.com/sensoryprocessingdisorderresources
Amazon offers a small commission on products sold through their affiliate links on my website. Each of your purchases through links on my website for Amazon affiliation links or sponsored links support me but no additional cost to you so thank you. I appreciate it so much! I am not responsible should you purchase anything from any links on this website.

Amazon
The Out-of-Sync Child
Amazon
Sensational Kids: Sensory Processing Disorder

Amazon
The Out-of-Sync Child Grows Up